The precarious work arrangements experienced by many long-term care workers have led to the creation of a “shared” workforce across residential, home, and community ageing care sectors. This shared workforce was identified as a contributor to the spread of COVID-19 early in the pandemic. The COVID-19 pandemic has disproportionately impacted residents and staff living and working in long-term care homes. Long-term care homes, commonly known as nursing homes or care homes, are facilities that primarily support ageing adults with functional, social and complex medical needs. By January 2021, long-term care residents accounted for a large proportion of COVID-19 deaths globally, making up an estimated 39% of deaths in the United States (US), 59% in Canada, 34% in the United Kingdom (UK) and 75% in Australia.
This analysis sought to review policy measures targeting the long-term care workforce across seven high-income jurisdictions during the first year of the COVID-19 pandemic. The focus was on financial supports introduced to recognize long-term care workers for the increased risks they faced, including both (1) health risks posed by direct care provision during the pandemic and (2) economic risks associated with restrictions to multi-site work.
Environmental scan of publicly available policy documents and government news releases published between March 1, 2020, and March 31, 2021, across seven high-income jurisdictions.
While there was limited use of financial measures in the United States to compensate long-term care workers for the increased health risks they faced, these measures were widely used across Canada, as well as in Wales, Scotland, and Australia. Moreover, there was a corresponding use of financial measures to protect workers from income loss in parts of Canada, Australia and the UK.
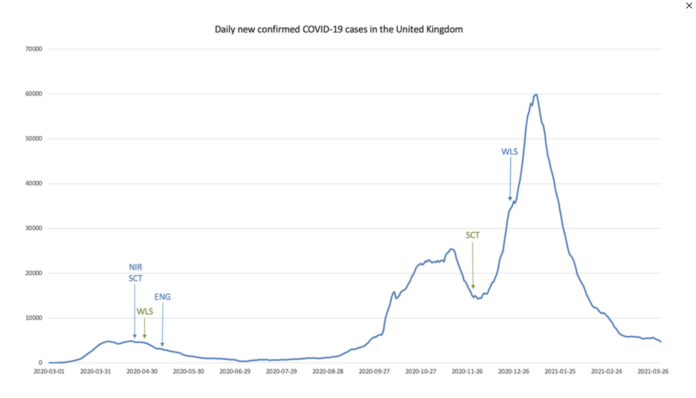
In the first year of the COVID-19 pandemic, policy measures were widely introduced in Canada and Australia in recognition of the increased risks faced by long-term care workers. In the UK, these were only introduced in Wales and Scotland, and in the US these measures were limited to only 11 states during the first year of the pandemic. In addition, there were widespread efforts taken to restrict multi-site work in Canada, the U.K, and Australia to limit virus transmission, though with the uneven implementation of corresponding economic protection measures to compensate long-term care workers for potential income loss. While these financial measures are temporary, they brought to light long-standing issues related to the supply of and support for workers providing care to older adults in long-term care homes. All seven jurisdictions in this study rely on long-term care workforces that are underpaid, often times precariously employed, and in some circumstances rely on multi-site work arrangements, yet the implementation of compensation and support has been uneven. In particular, there were considerable gaps in the US and parts of the UK in spite of considerably higher levels of risk overall as measured by population-level case counts and mortality than in Canada and Australia. Future studies should consider evaluating the impact of these measures and their effectiveness in reducing income loss among long-term care staff as a result of the pandemic.
Read the full publication:
Reed, A. C., Murmann, M., Hsu, A., Turnpenny, A., Van Houtven, C., Laberge, M.,Low, L.F., Hussein, S., Allin, S. (2022). Risk Recognition Policies for the Long-Term Care Workforce during the First Year of the COVID-19 Pandemic: A Multi-Country Study. Journal of Long-term Care, (2022), 22–39. DOI: http://doi.org/10.31389/jltc.110
Founder and Director
Shereen Hussein is a Health and Social Care Policy professor at the London School of Hygiene and Tropical Medicine (LSHTM), United Kingdom.
Shereen Founded the MENARAH Network in 2019, through an initial grant from the Global Challenge Research Fund, UKRI. She is a medical demographer with expertise in ageing, family dynamics, migration and long-term care systems. Shereen regularly collaborates with the United Nations, the World Health Organisation and the World Bank in policy and research focused on ageing in the Middle East and North Africa Region.
Shereen received her undergraduate degree in statistics and a postgraduate degree in computer science at Cairo University. She completed an MSc in medical demography at the London School of Hygiene and a PhD in quantitative demography and population studies at the London School of Economics and Political Science, United Kingdom.